

Type 1 diabetes, also known as juvenile or insulin-dependent , is a chronic autoimmune condition that affects individuals of all ages. Additionally, it occurs when the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. As a result, there is a deficiency of insulin, which is the hormone responsible for regulating blood sugar levels. Without adequate insulin, blood sugar levels can become dangerously high, leading to various health complications. In this article, we will delve into the symptoms, management, and advocacy efforts.
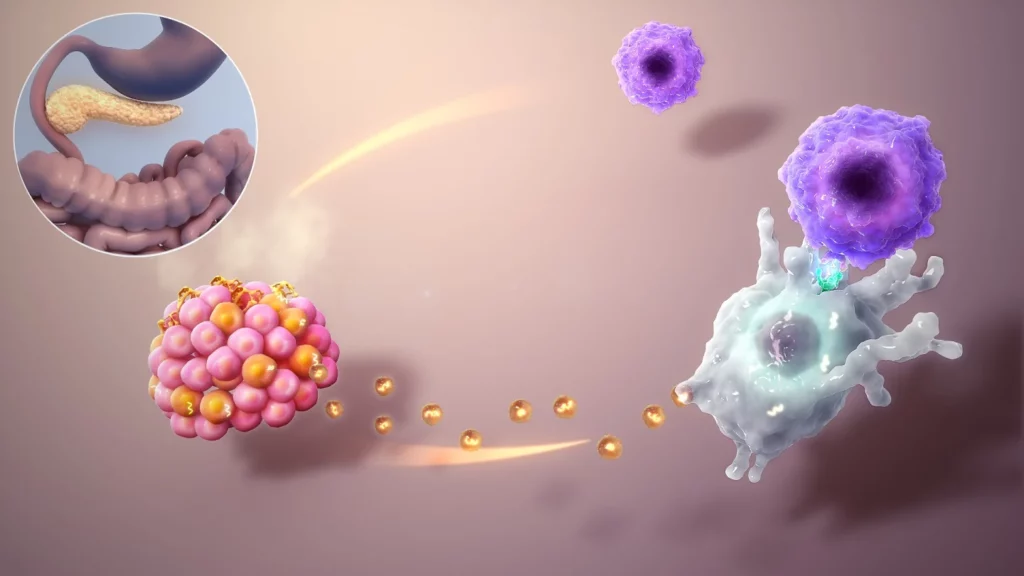
Type 1 diabetes is believed to have a complex interplay of genetic and environmental factors. Having a family history of the condition increases the risk of developing Type 1 diabetes, as well as exposure to certain environmental triggers such as viral infections, early childhood nutrition, and vitamin D deficiency.
Type 1 diabetes is usually diagnosed in children, adolescents, or young adults, although it can occur at any age. Common symptoms of Type 1 diabetes include frequent urination, excessive thirst, unexplained weight loss, increased hunger, fatigue, blurred vision, and slow healing of wounds. Diagnosis is typically confirmed through blood tests measuring blood glucose levels, HbA1c levels (a marker of average blood glucose levels over the past 2-3 months), and the presence of autoantibodies that attack the pancreatic beta cells.
Managing Type 1 diabetes requires a multi-faceted approach. It involves regular medical care, blood sugar monitoring, meal planning, physical activity, diabetes technology, psychosocial support, transitioning to adulthood, emergency preparedness, and advocacy efforts.
People with Type 1 diabetes need to pay careful attention to their diet and meal planning to manage blood sugar levels. This may involve counting carbohydrates, which are the main nutrient affecting blood sugar levels, and adjusting insulin doses accordingly. A registered dietitian or certified diabetes educator can provide personalized guidance on meal planning and help individuals with Type 1 diabetes make healthy food choices.
Regular physical activity is important for overall health and well-being, but it can also affect blood sugar levels in people with Type 1 diabetes. Exercise can cause blood sugar levels to drop, so it is important to monitor blood sugar levels before, during, and after physical activity and adjust insulin doses or carbohydrate intake as needed to prevent hypoglycemia.
In addition to insulin pumps and continuous glucose monitoring devices, there are other types of diabetes technology that can aid in the management of Type 1 diabetes. For example, insulin pens and jet injectors provide alternative methods for administering insulin, and smartphone apps and digital health platforms can help individuals with Type 1 diabetes track blood sugar levels, insulin doses, and other aspects of diabetes management.
Living with this aspects can have a significant impact on a person’s mental and emotional well-being. The constant monitoring, treatment regimen, and potential for complications can lead to stress, anxiety, depression, and diabetes distress. It is important to address the psychosocial aspects and seek support from healthcare professionals, counselors, or support groups to help cope with the emotional challenges associated with the condition.
Adolescents and young adults have to face unique challenges as they transition from pediatric to adult diabetes care. This may involve managing diabetes independently, dealing with changes in lifestyle and responsibilities, and navigating issues related to education, employment, relationships, and self-care. Transition programs and support from healthcare providers can assist in a smooth transition to adult diabetes care.
Advocacy efforts play a crucial role in improving the lives of individuals with Type 1 diabetes. This may involve raising awareness about the condition, advocating for policies that support access to affordable diabetes care and resources, and promoting research for new treatments and a cure. Participation in advocacy organizations and community initiatives can help individuals to make their voices heard and drive positive change.
Individuals need to be prepared for emergencies, such as severe hypoglycemia or diabetic ketoacidosis (DKA) – a life-threatening condition characterized by high blood sugar levels and a buildup of ketones in the blood. Having an emergency action plan, wearing medical alert identification, and carrying emergency supplies such as fast-acting carbohydrates and insulin can help individuals to manage emergencies effectively.
With ongoing research and advancements in diabete management, the future holds promise for individuals with Type 1 diabetes. Emerging technologies such as closed-loop systems, also known as artificial pancreas, hold the potential to automate insulin delivery and improve blood sugar control. Clinical trials exploring immunotherapies and other novel treatment approaches are also underway to potentially prevent .
Type 1 diabetes is a chronic autoimmune condition that requires lifelong management. It affects individuals of all ages and involves various aspects of daily life, including medical care, lifestyle modifications, emotional well-being, and advocacy efforts. With proper management and support, individuals can lead fulfilling lives and thrive despite the challenges posed by the condition. It is important to raise awareness, promote research, and advocate for policies that support individuals and improve their access to care and quality of life.